Abstract
Introduction: Patients with sickle cell disease frequently visit the emergency department and the most common reason for these visits is pain. Emergency department reliance (EDR) among the sickle cell population is an indicator of quality of care and access to outpatient settings. In the state of Wisconsin, more recent efforts to improve patient care include setting up a sickle cell clinic for adult patients, creating an electronic health records based registry for children with sickle cell disease, and expansion of hydroxyurea indication to all children ≥1 year of age with sickle cell anemia. There is a need to evaluate EDR for patients with sickle cell disease in the recent five years in order to inform stake holders of the impact of the invested efforts and also to identify potential areas for improvement. We hypothesize that EDR for pain has decreased over time in Wisconsin.
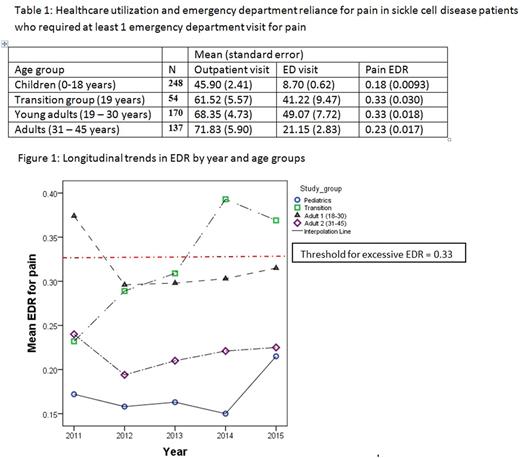
Methods: Using the Wisconsin state Medicaid data from years 2011 - 2015, we conducted a retrospective study to estimate EDR for patients with sickle cell disease and examined the trend of their EDR for pain over the period of 5 years. EDR identifies the proportion of emergency department visits among all ambulatory visits and is calculated as number of emergency department visits for pain divided by the number of emergency department visits for pain + outpatient visits. An EDR ≥ 0.33 has been previously identified as the threshold for excessive EDR. We a priori stratified the analyses by patient ages, categorized in four groups: 1) Children (age: 0 -18 years); 2) Transition group (those who turn 19 years old during the 5 year study period); 3) Young adults (age: 19 - 30 years); and 4) Adults (age: 31 - 45 years). The log transformed EDR was compared among the distinct four groups using analyses of variance. To identify the EDR trends over time, we used linear mixed model. The mixed model over time was adjusted for age group, adherence to hydroxyurea calculated as medication possession ratio (MPR) for hydroxyurea and interaction between covariates. MPR was a continuous variable in our model and calculated as sum of days hydroxyurea was supplied divided by the days enrolled minus the number of days hospitalized. Significance was set at p<0.05.
Results: The cohort included 609 sickle cell disease patients enrolled continuously in Wisconsin state Medicaid who had at least 1 sickle cell pain related emergency department visit. The average age of the cohort was 19 years in 2011. The overall EDR for pain in this cohort was 0.24 (SE = 0.0082). Table 1 shows the healthcare utilization and the pain EDR for each study group during the study period. The reliance on emergency department for patients in the transition group and young adults was significantly higher than children (p<0.001) and adults (p=0.0014 for transition and p <0.001 for young adults). EDR for children was significantly lower than adults older than 30 years of age (p = 0.0091). Longitudinal analyses show that EDR for pain has significantly different temporal patterns among groups (Figure 1), and an increase in MPR is associated with lower EDR. EDR for pediatrics has continually remained less than the established threshold of 0.33 though it significantly increased from 0.17 in 2011 to 0.21 in 2015 (p<0.001). The EDR for the transition group has been significantly increasing over time, however, in contrast, the EDR for young adults has significantly decreased since 2011 (p = 0.0013). There were no significant differences in EDR over time for adults older than 30 years.
Conclusion: The EDR for pain among children is below the threshold for excessive EDR and significantly lower than all other age groups, indicating the success of efforts vested for the pediatric population. In young adults, the pain EDR has significantly decreased since 2011. Unfortunately, the EDR for pain for patients in the transition age has been significantly increasing over time. Overall, a higher MPR suggesting adherence to hydroxyurea was associated with lower reliance on the ED for pain. Further interventions focusing on the transition age group are needed to improve care and ensure smooth transition from the pediatric to adult healthcare systems.
Panepinto: NIH: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal